Toenail fungus is a common and persistent problem that affects millions of people worldwide. It not only causes pain, discomfort, and embarrassment, but if left untreated, it may lead to serious complications such as permanent nail damage or spreading infections.
There are several different types of toenail fungus, each with unique characteristics and symptoms. Understanding them helps in proper diagnosis and treatment.
In this article, we’ll explore:
- What toenail fungus is
- Different types of toenail fungal infections
- Causes and risk factors
- Symptoms and warning signs
- Effective treatments and prevention strategies
Whether you have recently noticed early signs or have been struggling with toenail fungus for years, this guide will provide clear insights to help you manage and restore the health of your nails.
What is a Fungal Toenail Infection?
A fungal toenail infection (onychomycosis) is an infection that develops underneath the toenail, leading to:
- Nail discoloration (yellow, brown, white, or black)
- Thickening of the nail
- Brittleness and cracking
- Nail separation from the nail bed (onycholysis)
Toenails are more prone than fingernails because fungi thrive in warm, dark, moist environments—exactly what tight shoes and sweaty socks create.
This condition is persistent and hard to treat if not detected early. It is especially common in:
- Older adults
- Athletes
- People with weakened immune systems
- Those with poor foot hygiene or constant foot moisture exposure
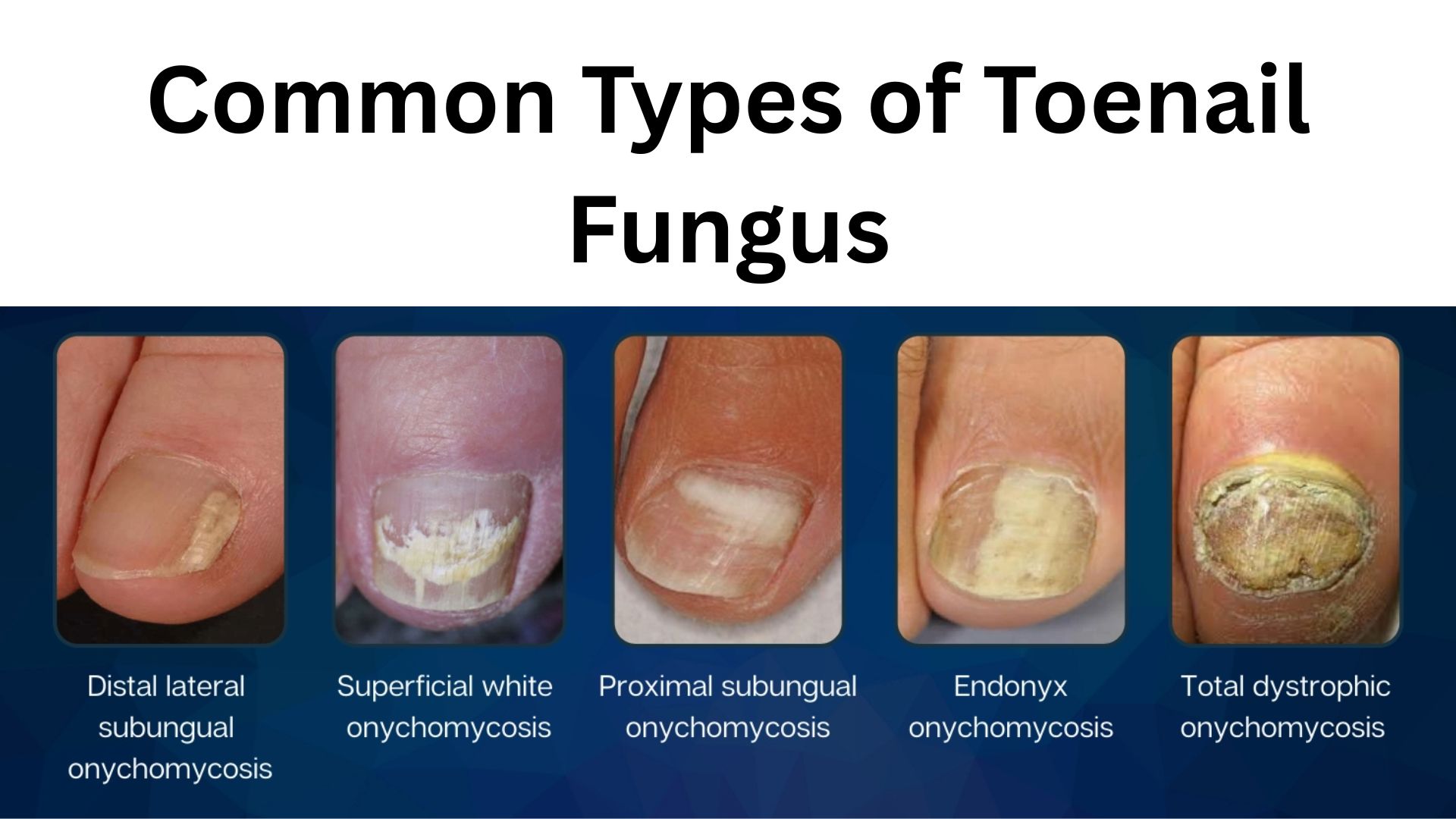
Common Types of Toenail Fungus
There are several types of fungal toenail infections, each with unique features:
1. Distal Subungual Onychomycosis (DSO)
- Most common form of toenail fungus.
- Caused by dermatophytes (fungi that feed on keratin).
- Starts at the tip of the nail and spreads inward.
- Symptoms: nail thickening, discoloration, brittle/crumbling edges, and detachment from the nail bed.
- Can be chronic and long-lasting if untreated.

DSO is the most common type of toenail fungal infection, causing thickened, discolored, and brittle nails starting from the tip of the nail
2. Superficial White Onychomycosis (SWO)
- Appears as white powdery patches or streaks on the nail surface.
- Fungi grow on top of the nail plate, unlike DSO which grows underneath.
- Usually painless, but nails become weak and crumbly.
- More common in toenails than fingernails.

SWO is a fungal infection that causes white spots or streaks on the nail surface, making the nail brittle and crumbly
3. Proximal Subungual Onychomycosis (PSO)
- Begins at the base of the nail (near cuticle) and spreads outward.
- Often affects people with weakened immune systems (e.g., diabetes, HIV).
- Nail becomes thick, discolored, and brittle.
- Early treatment is crucial to stop spreading.
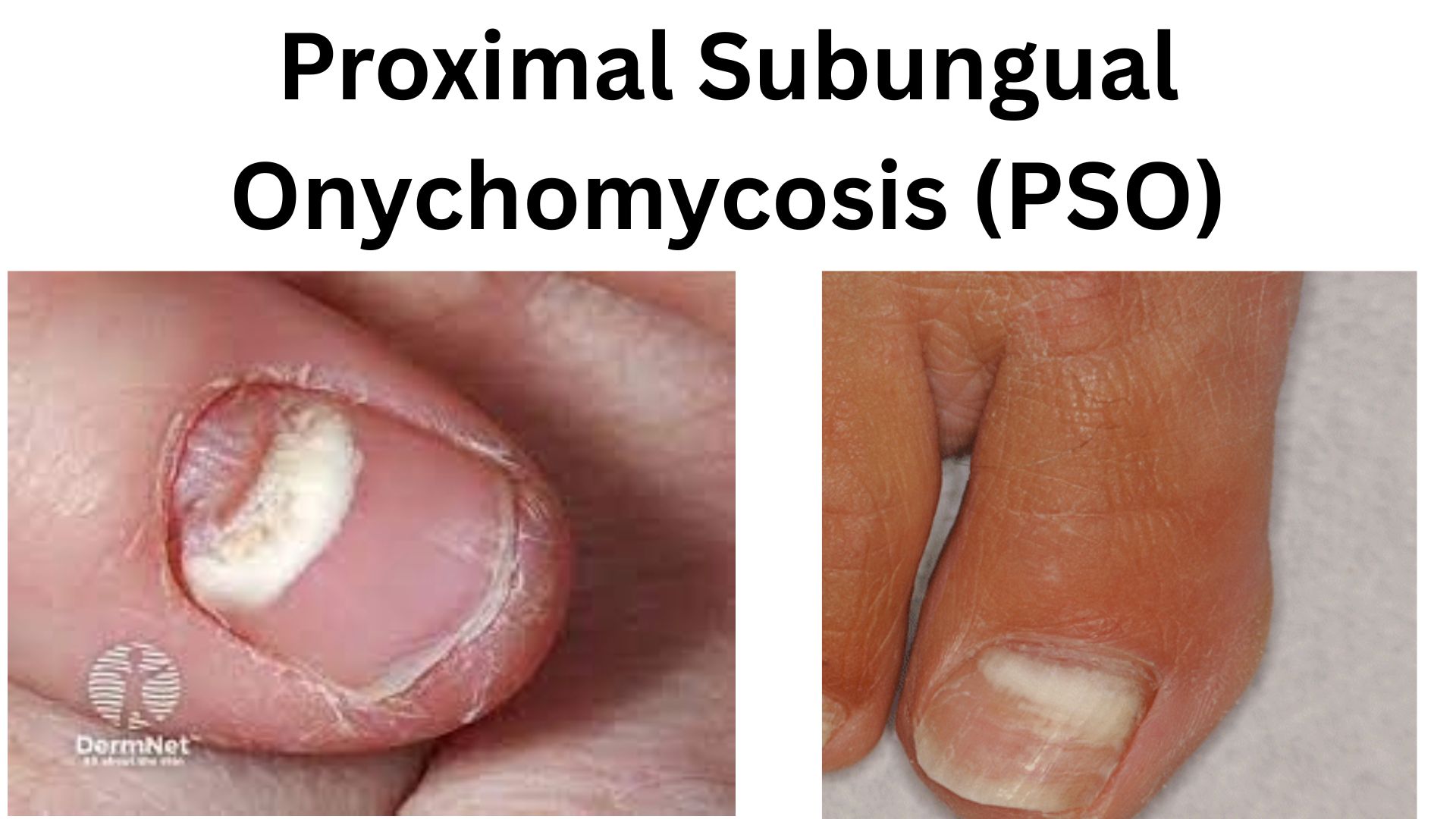
PSO is a fungal infection that begins at the base of the nail and spreads toward the tip, causing discoloration, thickening, and brittleness
4. Endonyx Onychomycosis
- Fungus primarily affects the nail bed (underneath the nail).
- Nail thickens, turns white or yellow, but surface changes are less visible.
- Difficult to diagnose without laboratory testing.

Endonyx Onychomycosis primarily affects the nail bed, causing subtle thickening and discoloration without significant surface changes
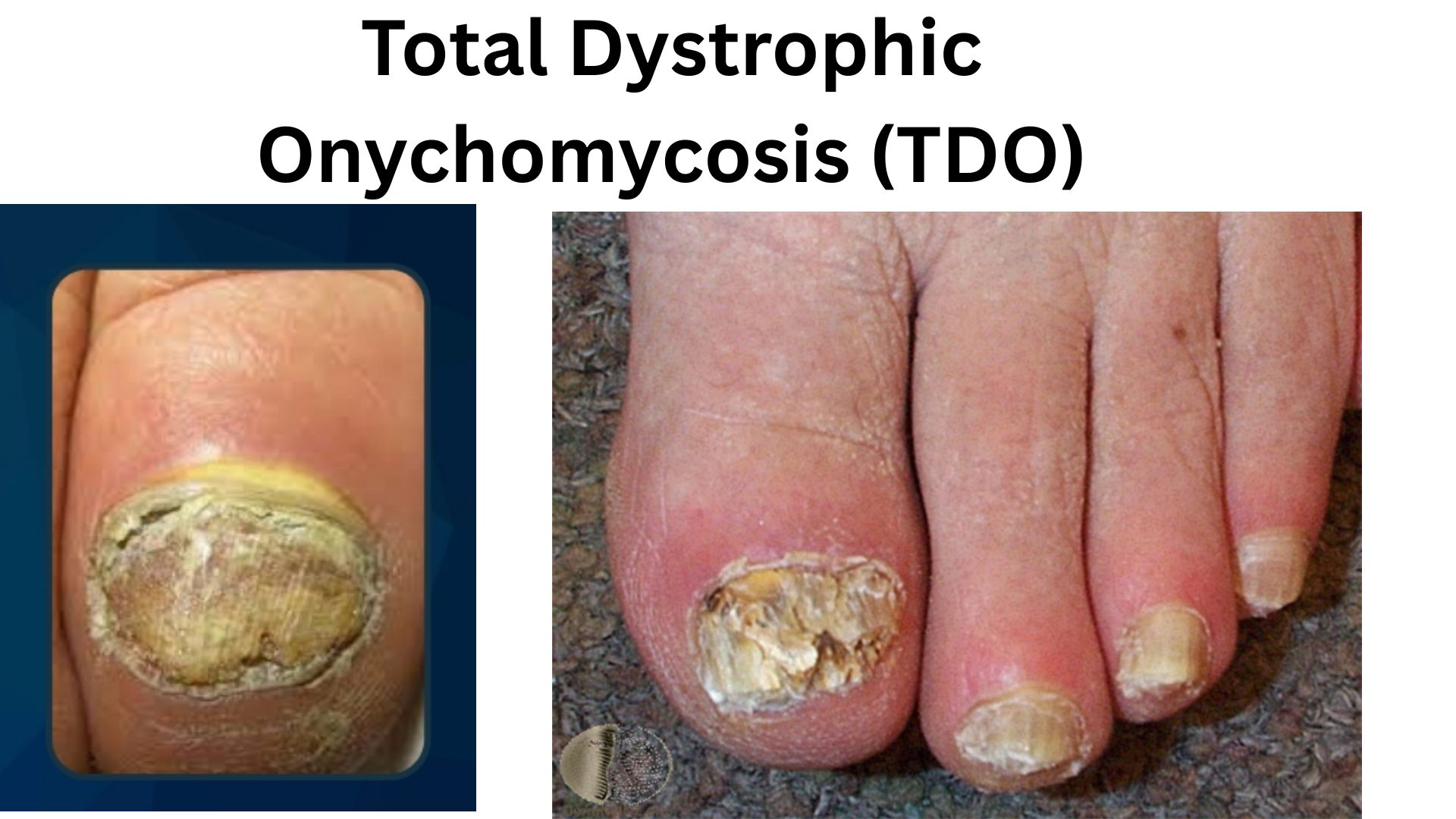
5. Total Dystrophic Onychomycosis (TDO)
- The end-stage of severe fungal infection.
- Results in complete destruction of the nail plate.
- Nail becomes thick, brittle, discolored, and may crumble completely.
- More common in people with diabetes, vascular disease, or poor immunity.
Signs and Symptoms of Toenail Fungus
Toenail fungal infections can look different depending on severity, but common signs include:
- Color changes: yellow, brown, white, or black patches.
- Thickening of the nail, making trimming difficult.
- Brittleness: nails break or crumble easily.
- Distorted nail shape (curved, twisted).
- Foul odor coming from the affected nail.
- Separation of the nail from the nail bed.
- Pain or discomfort while walking or wearing shoes.
👉 Not all cases show symptoms early on, which is why many infections go unnoticed until they worsen.
Causes and Risk Factors
Toenail fungus develops when fungi invade through tiny cracks or cuts in the nail or surrounding skin.
Common Causes:
- Dermatophytes (Trichophyton rubrum, Trichophyton mentagrophytes)
- Yeasts (Candida species)
- Non-dermatophyte molds
Risk Factors:
- Age: older adults have slower nail growth and reduced immunity.
- Nail trauma or injury.
- Frequent moisture exposure (swimmers, athletes).
- Poor hygiene or wearing tight, non-breathable shoes.
- Sharing shoes, socks, or nail tools.
- Underlying health issues: diabetes, peripheral artery disease, psoriasis.
- Weak immune system from chronic illnesses or medications.
- Athlete’s foot (tinea pedis) that spreads to toenails.
Prevention Strategies
Preventing toenail fungus is easier than treating it. Here are proven strategies:
- Wash feet daily with soap and dry thoroughly, especially between toes.
- Change socks daily; choose cotton or moisture-wicking fabrics.
- Wear breathable shoes and rotate pairs to let them dry.
- Avoid walking barefoot in public showers, pools, gyms.
- Keep toenails trimmed and clean.
- Use antifungal powders or sprays inside shoes.
- Disinfect nail clippers regularly.
- Do not share shoes, socks, or towels.
Treatment Options for Toenail Fungus
Treatment depends on the severity and type of fungus.
1. Home and Self-Care Remedies
- Keep nails short and filed.
- Use antifungal foot powders or sprays.
- Wear open-toed shoes when possible.
- Apply over-the-counter antifungal creams for mild infections.
2. Topical Medications
- Ciclopirox (nail lacquer)
- Amorolfine
- Antifungal creams/ointments (clotrimazole, terbinafine)
- Works better if the nail surface is thinned before application.
3. Oral Antifungal Medications
- Terbinafine (6–12 weeks) – high cure rate.
- Itraconazole – used in pulse therapy.
- Fluconazole – sometimes prescribed.
⚠️ Requires medical supervision due to possible liver side effects.
4. Advanced Options
- Laser therapy: kills fungus using light energy (costly but effective).
- Surgical removal of the infected nail (for severe cases).
- Chemical nail removal: using urea-based ointments.
When to See a Podiatrist or Doctor
Seek medical attention if:
- The infection is painful or spreading.
- You have diabetes, vascular disease, or weak immunity.
- Over-the-counter treatments don’t work.
- Multiple nails are infected.
- Nail is detaching or causing walking difficulty.
A podiatrist may perform:
- Nail examination
- Laboratory tests (KOH test, culture, biopsy)
- Tailored treatment plan
Complications of Untreated Toenail Fungus
Ignoring toenail fungus can lead to:
- Severe pain and discomfort
- Permanent nail deformity
- Spread to other nails and skin
- Secondary bacterial infections
- Serious foot complications in diabetic patients
Summary
Toenail fungus is a common but stubborn condition that requires timely attention. The major types include:
- Distal Subungual Onychomycosis
- Superficial White Onychomycosis
- Proximal Subungual Onychomycosis
- Endonyx Onychomycosis
- Total Dystrophic Onychomycosis
By understanding the causes, risk factors, and treatment options, you can take control of your nail health.
✅ Key Takeaways:
- Maintain good foot hygiene.
- Treat infections early to prevent complications.
- Seek medical care if symptoms persist or worsen.
With the right care, you can restore your nails and prevent future infections.
